Phoenix Children's Hospital may stop accepting one of nation's largest health insurers: 'Playing with lives'

Phoenix Children's to drop UnitedHealthcare
Today could be the final day that Phoenix Children's Hospital accepts United Healthcare. Earlier this month, the hospital announced that UCH would no longer be an in-network provider if a deal couldn't be reached by May 31.
PHOENIX - The Phoenix Children's Hospital has told families they may no longer accept UnitedHealthcare insurance by June 1, causing panic for parents with kids battling long-term illnesses.
On Monday, the hospital announced that UnitedHealthcare may no longer be an in-network provider if a new deal is not reached between the two entities. Coverage would end May 31 for employer-sponsored and individual commercial plans.
"UnitedHealthcare Community Plan in Arizona (Medicaid) members are not impacted by this negotiation and will remain in network through a separate agreement," said Catherine Farrell with UHC.
Hospital officials said they wanted to give everyone as much notice as possible to avoid disruptions.
For families with UnitedHealthcare as their insurer, it's a scary and stressful waiting game to see if they have to find somewhere else to be treated.
‘Playing with lives’

Phoenix Children's says UnitedHealthcare will not be accepted by June
Valley families have panicked since Monday over health insurance. Phoenix Children’s told families saying they may no longer accept UnitedHealthcare insurance starting June 1. For parents with kids battling long-term illnesses, that’s a shock. FOX 10's Steve Nielsen has more on how these negotiations are impacting kids.
Every few months, 8-year-old Brock comes to Phoenix Children's to get an MRI. The last one was bad news: the tumor wrapped around his optical nerve started growing again.
"Inoperable," said his father, Eric Koziatek. "Can't biopsy it. You risk blinding him."
After 18 months of chemotherapy, it had finally frozen its size. But since recent tests show it's growing again, he may have to start chemo all over again if another MRI later this month continues to show that.
"He pushed it out of his mind and was back to a kid," said Koziatek. "And facing the prospect of doing it all again for us is hard, I can’t imagine what he feels."
It's an unimaginable stress for the Chandler family, but it only got worse Monday.
Eric's health insurance? United.
"Honestly the range of emotions that ran through me when I saw that were very similar to when I first found out my kid had a tumor," said Koziatek.
Eric says his son developed a bond with his doctor.
"He got to a point where he was laughing and joking with his doctor he would put a fake mustache on and scare him when he came in the room," Koziatek said. "They’ve got that bond, patient and doctor in addition to parent [and] doctor…trying to foster that same thing with someone from scratch is going to be tough.
"You're not just playing with money," the 8-year-old's father continued. "You're playing with lives."
Negotiations
KFF, an independent nonprofit focused on national health issues, says these negotiations come down to rates.
"If insurers want to drive down health care costs and premiums, they have to appear and be willing to walk away if they’re not going to get the rates they’re looking for," said Krutika Amin with KFF.
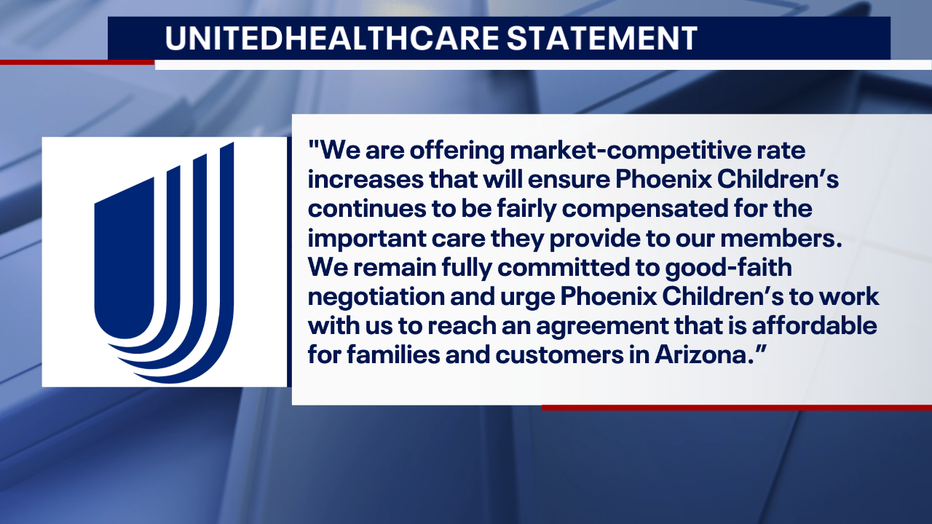
UnitedHealthcare says they’re offering market competitive rate increases, and released the following statement:
"We remain fully committed to good-faith negotiation and urge Phoenix Children’s to work with us to reach an agreement that is affordable for families and customers in Arizona."
Options for affected families
According to UnitedHealthcare representative Catherine Farrell, there are still options available for affected families if negotiations fall through.
Members who are in the middle of treatment at Phoenix Children's may qualify for continuity of care, which provides in-network benefits for a set period of time after the hospital leaves the network.
"In the event PCH leaves our network, we are committed to collaborating with the health system to help ensure the children and families we serve experience a smooth transition to a new provider, as appropriate," said Farrell in a statement. "For children battling chronic medical conditions such as cancer, we will work with PCH to help ensure they have continued access to the care they need at PCH through continuity of care."
The insurance provider has reportedly reached out to Brock's family to inform them about continuity of care.
"Children like Brock, who are in the middle of treatment for a chronic condition, may qualify for Continuity of Care and will continue to have access to the doctors and the care they need at Phoenix Children’s, in the event it should go out of network," Farrell said.
Anyone with questions about qualifying for coverage can call the number on their health plan card for assistance.

